Difference between revisions of "Motion artifact reduction for reflection mode photoplethysmography"
m (Placeholder (to make a permalink)) |
(Added publication (Motion limitations of non-contact...)) |
||
| (3 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
| − | + | __NOTOC__ | |
| + | |||
| + | |||
| + | = Motion artifact reduction for reflection mode photoplethysmography = | ||
| + | |||
| + | '''Student:''' [[Matthew Butler]] | ||
| + | |||
| + | '''Supervisors:''' [[Barrie Hayes-Gill]], [[John Crowe]], [[Paul Rodmell]] | ||
| + | |||
| + | The primary objective is to reduce the effects of motion on the photoplethysmogram. Through the project, multiple 'types' of photoplethysmography will be considered (transmission- and reflection- mode, in- and non- contact), however the final aim will be to target just in-contact reflection-mode photoplethysmography. | ||
| + | |||
| + | == Motivation == | ||
| + | Approximately one tenth of all newborns require some form of resuscitation after birth. During the resuscitation, one of the most critical vital signs, the heart-rate, is used as an indication of the success of the procedure. The current method of measuring the heart-rate is for the clinicians to use a stethoscope and count the beats in a six or ten second window, multiplying the result appropriately to get beats per minute (bpm). The disadvantage with this method is that during the heart-beat counting, resuscitation cannot be taking place - vital time is being lost. | ||
| + | |||
| + | Traditional electrocardiography (ECG) is not suitable for use with newborns for three main reasons. Firstly, the preparation time for even a three-point ECG is long as the skin needs to be prepared before the electrodes are placed. As the newborn has just emerged from their mother's womb, they are covered in vernix, blood and other fluids that would prevent the electrodes from making sufficient contact. Secondly, as soon as resuscitation is found to be required, the newborn in placed in a plastic bag up to their neck to prevent a loss of heat. The audio based stethoscopes will work through the thin material, but ECG will not. Again attempting to clean the skin and position the electrodes through the opening of the bag, whilst not losing much heat, is impracticable. And lastly, newborns' skin is very weak and prone to damage, so attaching ECG electrodes to the skin via self-adhesive pads or medical tape may cause irreparable damage. | ||
| + | |||
| + | Photoplethysmography (PPG), being an optical technique, could work through a transparent wrap, however, conveniently, as a PPG signal can be obtained from anywhere on the surface of the skin, the forehead is a good choice. Not only does it have a relatively high blood perfusion, making the detection of the pulsatile signal easier, but the forehead is not within the confines of the plastic bag so easy access is possible. Additionally, PPG will work through the thin layer of fluids and vernix that is on the newborn's skin. This may attenuate the signal slightly, but will not interfere with the 'AC' component that is the PPG. One final convenience of choosing the forehead to perform the PPG measurement on is that as well as the plastic bag to keep the body warm, the newborn's head is fitted with a hat for the same reason. As PPG sensors can be made small, the sensor head can be part of the hat, potentially woven into the material. | ||
| + | |||
| + | The main disadvantage of PPG, however, is it susceptibility to movement. During resuscitation, there will be movement that may corrupt the PPG. It is this hurdle that is being researched in this project. | ||
| + | |||
| + | == Background == | ||
| + | |||
| + | === Photoplethysmography === | ||
| + | ''Main article: [https://en.wikipedia.org/wiki/Photoplethysmogram Photoplethysmography]'' | ||
| + | |||
| + | Photoplethysmography (PPG) is a technique that uses light to measure the cardiac-synchronous pulsations of the blood around the body. This is possible due to the optical interactions with the blood beneath the skin and the highly scattering nature of the tissue. By shining a light source at the skin and detecting the fluctuating light intensities that re-emerge from it, the photoplethysmogram (also acronymised PPG) can be obtained. By utilising multiple wavelengths of light, it is possible to perform pulse oximetry, where an estimation of the oxygen content of the blood can be made. However, the heart-rate is the simplest vital metric to be calculated and is often the most useful in both clinical and commercial (fitness) settings. | ||
| + | |||
| + | === Motion Artifacts === | ||
| + | Photoplethysmography is highly prone to errors caused by movement of the light source-sensor relative to the subject-under-test. There are several reasons for these artifacts, but most can be explained by the additional attenuation of the signal caused by either the optical path between the source and sensor changing position and passing through different tissue structures, or changing length, in which case the light will be attenuated (by absorption) by differing amounts. | ||
| + | |||
| + | Due to the unpredictability of human motion, the fact that the mechanical motion is not directly related to the optical effect that is observed, and that typical artifacts have similar frequency components to that of the PPG, motion artifacts are particularly difficult to overcome. | ||
| + | |||
| + | == Previous Research == | ||
| + | Previous researchers have attempted to solve the 'motion artifact problem' with a variety of techniques. These techniques range from simple mechanical adjustments to standard sensors, to adaptive filtering techniques, to using multiple wavelengths to try to extract the motion separately, to complex post-processing algorithms that attempt reconstruction of the PPG. Whilst many have shown some improvement in the PPG signal either in very specific circumstances or under laboratory conditions, there has been little research published that claims to solve the problem for practical 'real-world' applications. | ||
| + | |||
| + | == Methodology == | ||
| + | As opposed to many of the previous research projects which looked into modelling the optical systems associated with photoplethysmography, or looked at controlling the environment to create reproducible laboratory conditions, this project took a more empirical approach to solving the problem. This was mainly due to the random biological nature of the human body and it movements; it was believed that any attempt to model the ever-changing optical properties of the body would be nearly impossible for the given project duration, and then there would be no guarantee that a solution existed for that particular model. | ||
| + | |||
| + | By observing the effects of motion on the PPG signal itself, rather than attempting to measure the motion separately (as many other have tried) and 'subtracting' it from the measured signal, it was possible to determine the cause of the artifacts ''as seen by the photo-detector''. | ||
| + | |||
| + | After looking at many aspects of photoplethysmography, both old and new, a device was designed that was a combination of a novel sensor head, bespoke electrical circuitry and streaming processing. The design used redundancy in information gathered from a sensor array to compensate for motion artifacts. It was discovered that the artifacts are not always evenly distributed across the surface of a sensor; by having multiple detection elements in a patterned array, a PPG can be calculated where it would not be possible with just a single element. | ||
| + | |||
| + | This design has been tested preliminarily using a desktop mounted (ie. not portable) set-up with promising results. Additionally to this test, a simpler, portable design was created that incorporated additional sensors, specifically ECG and accelerometers, to test the effectiveness of the algorithms that were designed. | ||
| + | |||
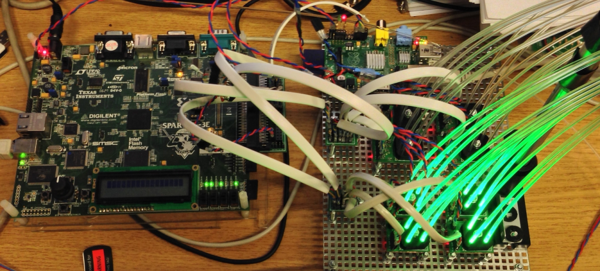
| + | [[File:mjb_optical_matrix.png|600px|thumb|center|Desktop 'optical matrix' PPG sensor.]] | ||
| + | |||
| + | === Novelty === | ||
| + | The true novelty of this design comes from the source/sensor array which is fundamental to the functionality of the system. There have not been (to date) any publications seen that use a system like this for photoplethysmogrpahy. Due to the extra data that is output from the unique sensor design, the processing is also new. Although its roots lie in other techniques, the processing stage is fundamentally new. | ||
| + | |||
| + | === Trials === | ||
| + | Two participant trials have taken place in the project's duration, each with the appropriate ethics approval. | ||
| + | :1. ''Heart-rate detection using a camera: experiment on limitations.'' | ||
| + | :: The intention of this trial was to collect data from participants to evaluate the theoretical limitations of using imaging photoplethysmography to extract the heart-rate. | ||
| + | :2. ''Photoplethysmography/Electrocardiography: Algorithm validation.'' | ||
| + | :: This trial was used to validate algorithms that will be used in the final design that determine the 'quality' of a PPG signal without addition cardiac information. | ||
| + | |||
| + | === Publications === | ||
| + | ''[[Matthew Butler]], [[John Crowe]], [[Barrie Hayes-Gill]] and [[Paul Rodmell]],'' [http://iopscience.iop.org/article/10.1088/0967-3334/37/5/N27 Motion limitations of non-contact photoplethysmography due to the optical and topological properties of skin], [http://iopscience.iop.org/journal/0967-3334 Physiological Measurement] '''37''' N27 (2016) | ||
| + | |||
| + | == End Goal == | ||
| + | The final goal of the project is to create a fully working, portable, system that incorporates all of the prior research. The intention is to directly compare the output from the system with the output from the leading 'competitor' during natural behavioural movement. | ||
| + | |||
| + | == Links with Industry == | ||
| + | This PhD project, initially funded by the EPSRC was converted to a CASE award through Tioga Ltd., an electronics manufacturing company based in Derby, UK. From October 2015, Matthew began to work at Tioga part-time whilst he completed his PhD. His primary role is as an electronics/firmware engineer on the 'HeartLight' project, but also works on other projects within the company. | ||
| + | |||
| + | HeartLight Systems Ltd. is a company that was set up as a joint venture between Tioga and the University of Nottingham, and are currently (2015/2016) developing a device specifically for use during newborn resuscitation. There is potential in the future for the the research outcomes from this project to be incorporated into the HeartLight device. | ||
Latest revision as of 15:46, 27 April 2016
Motion artifact reduction for reflection mode photoplethysmography
Student: Matthew Butler
Supervisors: Barrie Hayes-Gill, John Crowe, Paul Rodmell
The primary objective is to reduce the effects of motion on the photoplethysmogram. Through the project, multiple 'types' of photoplethysmography will be considered (transmission- and reflection- mode, in- and non- contact), however the final aim will be to target just in-contact reflection-mode photoplethysmography.
Motivation
Approximately one tenth of all newborns require some form of resuscitation after birth. During the resuscitation, one of the most critical vital signs, the heart-rate, is used as an indication of the success of the procedure. The current method of measuring the heart-rate is for the clinicians to use a stethoscope and count the beats in a six or ten second window, multiplying the result appropriately to get beats per minute (bpm). The disadvantage with this method is that during the heart-beat counting, resuscitation cannot be taking place - vital time is being lost.
Traditional electrocardiography (ECG) is not suitable for use with newborns for three main reasons. Firstly, the preparation time for even a three-point ECG is long as the skin needs to be prepared before the electrodes are placed. As the newborn has just emerged from their mother's womb, they are covered in vernix, blood and other fluids that would prevent the electrodes from making sufficient contact. Secondly, as soon as resuscitation is found to be required, the newborn in placed in a plastic bag up to their neck to prevent a loss of heat. The audio based stethoscopes will work through the thin material, but ECG will not. Again attempting to clean the skin and position the electrodes through the opening of the bag, whilst not losing much heat, is impracticable. And lastly, newborns' skin is very weak and prone to damage, so attaching ECG electrodes to the skin via self-adhesive pads or medical tape may cause irreparable damage.
Photoplethysmography (PPG), being an optical technique, could work through a transparent wrap, however, conveniently, as a PPG signal can be obtained from anywhere on the surface of the skin, the forehead is a good choice. Not only does it have a relatively high blood perfusion, making the detection of the pulsatile signal easier, but the forehead is not within the confines of the plastic bag so easy access is possible. Additionally, PPG will work through the thin layer of fluids and vernix that is on the newborn's skin. This may attenuate the signal slightly, but will not interfere with the 'AC' component that is the PPG. One final convenience of choosing the forehead to perform the PPG measurement on is that as well as the plastic bag to keep the body warm, the newborn's head is fitted with a hat for the same reason. As PPG sensors can be made small, the sensor head can be part of the hat, potentially woven into the material.
The main disadvantage of PPG, however, is it susceptibility to movement. During resuscitation, there will be movement that may corrupt the PPG. It is this hurdle that is being researched in this project.
Background
Photoplethysmography
Main article: Photoplethysmography
Photoplethysmography (PPG) is a technique that uses light to measure the cardiac-synchronous pulsations of the blood around the body. This is possible due to the optical interactions with the blood beneath the skin and the highly scattering nature of the tissue. By shining a light source at the skin and detecting the fluctuating light intensities that re-emerge from it, the photoplethysmogram (also acronymised PPG) can be obtained. By utilising multiple wavelengths of light, it is possible to perform pulse oximetry, where an estimation of the oxygen content of the blood can be made. However, the heart-rate is the simplest vital metric to be calculated and is often the most useful in both clinical and commercial (fitness) settings.
Motion Artifacts
Photoplethysmography is highly prone to errors caused by movement of the light source-sensor relative to the subject-under-test. There are several reasons for these artifacts, but most can be explained by the additional attenuation of the signal caused by either the optical path between the source and sensor changing position and passing through different tissue structures, or changing length, in which case the light will be attenuated (by absorption) by differing amounts.
Due to the unpredictability of human motion, the fact that the mechanical motion is not directly related to the optical effect that is observed, and that typical artifacts have similar frequency components to that of the PPG, motion artifacts are particularly difficult to overcome.
Previous Research
Previous researchers have attempted to solve the 'motion artifact problem' with a variety of techniques. These techniques range from simple mechanical adjustments to standard sensors, to adaptive filtering techniques, to using multiple wavelengths to try to extract the motion separately, to complex post-processing algorithms that attempt reconstruction of the PPG. Whilst many have shown some improvement in the PPG signal either in very specific circumstances or under laboratory conditions, there has been little research published that claims to solve the problem for practical 'real-world' applications.
Methodology
As opposed to many of the previous research projects which looked into modelling the optical systems associated with photoplethysmography, or looked at controlling the environment to create reproducible laboratory conditions, this project took a more empirical approach to solving the problem. This was mainly due to the random biological nature of the human body and it movements; it was believed that any attempt to model the ever-changing optical properties of the body would be nearly impossible for the given project duration, and then there would be no guarantee that a solution existed for that particular model.
By observing the effects of motion on the PPG signal itself, rather than attempting to measure the motion separately (as many other have tried) and 'subtracting' it from the measured signal, it was possible to determine the cause of the artifacts as seen by the photo-detector.
After looking at many aspects of photoplethysmography, both old and new, a device was designed that was a combination of a novel sensor head, bespoke electrical circuitry and streaming processing. The design used redundancy in information gathered from a sensor array to compensate for motion artifacts. It was discovered that the artifacts are not always evenly distributed across the surface of a sensor; by having multiple detection elements in a patterned array, a PPG can be calculated where it would not be possible with just a single element.
This design has been tested preliminarily using a desktop mounted (ie. not portable) set-up with promising results. Additionally to this test, a simpler, portable design was created that incorporated additional sensors, specifically ECG and accelerometers, to test the effectiveness of the algorithms that were designed.
Novelty
The true novelty of this design comes from the source/sensor array which is fundamental to the functionality of the system. There have not been (to date) any publications seen that use a system like this for photoplethysmogrpahy. Due to the extra data that is output from the unique sensor design, the processing is also new. Although its roots lie in other techniques, the processing stage is fundamentally new.
Trials
Two participant trials have taken place in the project's duration, each with the appropriate ethics approval.
- 1. Heart-rate detection using a camera: experiment on limitations.
- The intention of this trial was to collect data from participants to evaluate the theoretical limitations of using imaging photoplethysmography to extract the heart-rate.
- 2. Photoplethysmography/Electrocardiography: Algorithm validation.
- This trial was used to validate algorithms that will be used in the final design that determine the 'quality' of a PPG signal without addition cardiac information.
Publications
Matthew Butler, John Crowe, Barrie Hayes-Gill and Paul Rodmell, Motion limitations of non-contact photoplethysmography due to the optical and topological properties of skin, Physiological Measurement 37 N27 (2016)
End Goal
The final goal of the project is to create a fully working, portable, system that incorporates all of the prior research. The intention is to directly compare the output from the system with the output from the leading 'competitor' during natural behavioural movement.
Links with Industry
This PhD project, initially funded by the EPSRC was converted to a CASE award through Tioga Ltd., an electronics manufacturing company based in Derby, UK. From October 2015, Matthew began to work at Tioga part-time whilst he completed his PhD. His primary role is as an electronics/firmware engineer on the 'HeartLight' project, but also works on other projects within the company.
HeartLight Systems Ltd. is a company that was set up as a joint venture between Tioga and the University of Nottingham, and are currently (2015/2016) developing a device specifically for use during newborn resuscitation. There is potential in the future for the the research outcomes from this project to be incorporated into the HeartLight device.